Overview
The Bariatric Surgery Department specializes in surgical treatments for obesity and related health conditions. Our experienced team of surgeons, dietitians, and support staff provides comprehensive care to help patients achieve significant weight loss and improve their overall health. Bariatric surgery is not just about losing weight; it’s about enhancing quality of life by reducing the risk of obesity-related diseases such as diabetes, hypertension, and sleep apnea. We offer a range of minimally invasive procedures tailored to each patient’s unique needs, ensuring safe and effective outcomes.
TREATMENTS & PROCEDURE

A surgical procedure that changes how your stomach and small intestine handle food for effective weight loss.
Gastric bypass surgery involves creating a small pouch from the stomach and connecting it directly to the small intestine. This reduces the amount of food you can eat and decreases calorie absorption, leading to significant weight loss.

A minimally invasive procedure that removes a portion of the stomach to limit food intake.
Sleeve gastrectomy involves removing a large part of the stomach, leaving a tube-like structure. This limits the amount of food you can eat and helps reduce hunger hormones, promoting effective weight loss.

A procedure that places an adjustable band around the upper part of the stomach to control food intake.
Adjustable gastric banding involves placing a silicone band around the upper part of the stomach to create a small pouch. The band can be adjusted to control the rate of weight loss and help patients manage their appetite effectively.

An extensive procedure that reduces stomach size and bypasses part of the small intestine.
This procedure involves removing a portion of the stomach and bypassing a significant part of the small intestine. It reduces food intake and calorie absorption, making it effective for patients with severe obesity.
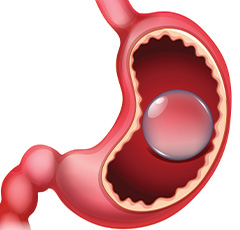
A temporary, non-surgical procedure involving the placement of a balloon in the stomach.
The intragastric balloon procedure involves placing a silicone balloon in the stomach, which is then filled with saline. This helps patients feel full sooner and eat less, promoting weight loss. The balloon is typically removed after six months.

Procedures to revise or correct previous bariatric surgeries for improved outcomes.
Revisional bariatric surgery addresses complications or inadequate weight loss from previous surgeries. It involves modifying or converting the original procedure to achieve better results and enhance patient health.
A surgical procedure that changes how your stomach and small intestine handle food for effective weight loss.

Gastric bypass surgery involves creating a small pouch from the stomach and connecting it directly to the small intestine. This reduces the amount of food you can eat and decreases calorie absorption, leading to significant weight loss.
A minimally invasive procedure that removes a portion of the stomach to limit food intake.

Sleeve gastrectomy involves removing a large part of the stomach, leaving a tube-like structure. This limits the amount of food you can eat and helps reduce hunger hormones, promoting effective weight loss.
A procedure that places an adjustable band around the upper part of the stomach to control food intake.

Adjustable gastric banding involves placing a silicone band around the upper part of the stomach to create a small pouch. The band can be adjusted to control the rate of weight loss and help patients manage their appetite effectively.
An extensive procedure that reduces stomach size and bypasses part of the small intestine.

This procedure involves removing a portion of the stomach and bypassing a significant part of the small intestine. It reduces food intake and calorie absorption, making it effective for patients with severe obesity.
A temporary, non-surgical procedure involving the placement of a balloon in the stomach.
The intragastric balloon procedure involves placing a silicone balloon in the stomach, which is then filled with saline. This helps patients feel full sooner and eat less, promoting weight loss. The balloon is typically removed after six months.
Procedures to revise or correct previous bariatric surgeries for improved outcomes.

Revisional bariatric surgery addresses complications or inadequate weight loss from previous surgeries. It involves modifying or converting the original procedure to achieve better results and enhance patient health.
Diseases treated
FAQs
Bariatric surgery includes procedures that help with weight loss by restricting the amount of food the stomach can hold or by limiting calorie absorption. It’s effective for severe obesity.
Recovery time varies by procedure, but most patients can return to normal activities within 2-4 weeks. Full recovery and adjustment to a new diet can take several months.
Weight loss varies by procedure and individual, but most patients lose 50-70% of their excess weight within the first two years after surgery.
Dietitians provide essential support before and after surgery, helping patients follow dietary guidelines, manage nutritional intake, and make lifestyle changes for successful weight loss.
Candidates typically have a BMI of 40 or higher, or a BMI of 35-39.9 with obesity-related health conditions like diabetes or hypertension. A thorough medical evaluation is required.
Risks include infection, blood clots, and complications related to anesthesia. Long-term risks can include nutritional deficiencies, so ongoing medical follow-up is essential.
Yes, a specific diet is required post-surgery, starting with liquids and gradually progressing to solid foods. Long-term dietary changes are essential for maintaining weight loss.
Bariatric surgery can significantly improve or even resolve type 2 diabetes in many patients by promoting weight loss and improving insulin sensitivity. However, individual results vary.
Bariatric Surgery Doctors




Dr. Najla Mohammed Rashid Alghaiti
Senior specialist- General and Laparoscopic Surgery (Visiting consultant)










